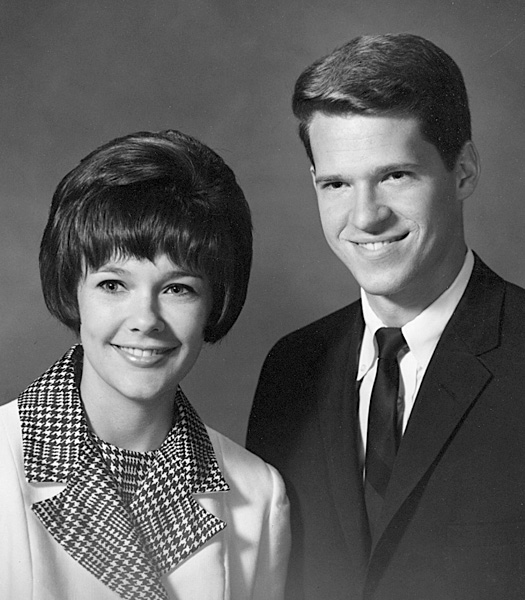
Rebecca and Michael engagement photo May 20, 1966
Life is short, the art long, opportunity fleeting,
experiment treacherous, judgment difficult.
(attributed to Hippocrates)
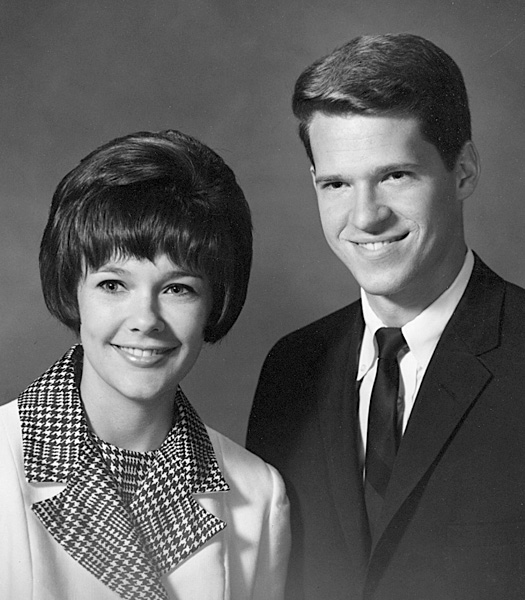
Rebecca and Michael engagement photo May 20, 1966
I felt fortunate to get into Baylor University College of Medicine (BUCM or BCM, also loosely called "Baylor Medical School", or just "Baylor Med" for short). It was just across the street from Rice University in Houston, Texas, and attending it did not compel me to uproot my lifestyle or even so much as move my lodgings. (Baylor Med is not near its Baptist former parent organization, Baylor University, which is in Waco, Texas. In fact, Baylor Med was in the process of disaffiliating from Baylor University, in order to qualify for federal research funds and to broaden its nonsectarian support. The final separation was completed in 1969, at which time its official name became and remains Baylor College of Medicine). The Texas Medical Center, in which BCM is located, was already a major and extraordinarily burgeoning complex devoted to medical education, research, and patient care, and offered plenty for the aspiring future physician to take inspiration from. Incredibly, this medical center is almost unrecognizable to me now as a result of the astounding growth it has continued to exhibit over the years. When I attended BCM, there were already numerous institutions on or near the Texas Medical Center campus with which BCM was actively affiliated: Ben Taub General Hospital, the VA Hospital, St. Luke's Hospital, Methodist Hospital, Texas Children's Hospital, and many others.
Looking over the school annual from 1966, the Aesculapian (see Ref. 2 regarding the origin of this name), I note that our MD-candidate class had about 85 freshmen, about 1/3 of which had graduated from Texas colleges. (Unlike my Rice annuals, my photo appears in all four year's Aesculapians—I could no longer lurk in obscurity.) This was an era at Baylor and elsewhere when the MD students were still overwhelmingly white and male, but three intrepid bright women were also included in my class along with one black male and one Asian male (from Hong Kong). The flexible academic tracks allowed students to take off a year or more to study in the basic sciences such as anatomy and physiology, so my class had individuals leaving and rejoining throughout the four years I was there. In addition, there was a substantial contingent at BCM of excellent non-MD-track graduate students (e.g., in pharmacology, physiology, etc.) who added to the scientific biodiversity of the school. (Hereafter, however, when I refer to fellow students, I will be simply referring to my MD-track classmates.)
Dr. James R. Schofield was a major figure from my BCM years, a BCM graduate himself in the class of '47. At the time he was the Dean of Academic Affairs and the leadership figure with whom the students had the greatest contact. I recall the tone he set for his medical students very well. He was a neat and trim person himself, and he expected appropriate attire and a sense of decorum in his students. While this might come to seem a little old-fashioned and stuffed-shirt in ensuing decades, I can recall how many times I saw patients in later years who were dismayed or confused by the unkempt appearance of students and house staff—they could sometimes not be distinguished from vagrants off the street. He insisted that we wear clean dress shirts, tie, slacks, and dress shoes (though conceding that in the Texas heat, a coat was not usually required). This became my medical uniform that carried me through my career (invariably short sleeve shirts even in the cold North, in view of the messes I frequently had to get my gloved hands into). The Schofield look produced a somewhat bland uniformity of appearance, like at a Catholic school, but we were able to focus on getting the task of learning medicine done, and I believe the patients appreciated the image we cultivated. Dr. Schofield set a high standard of behavior as well as of dress, and was an inspiration to me. If I recall correctly, he was unmarried and childless and seemed to regard his students like a large extended family.
How BCM Regarded Its Medical Students: Being in medical school was quite unlike being at Rice. In contrast to the sink-or-swim indifference I seemed to encounter at Rice (where eligible student candidates were a dime-a-dozen and could easily be replaced), BCM was investing substantial resources in its much smaller class of medical students. It was clear to me that they actually wanted us to survive the difficult curriculum and to become physicians—and they were genuinely focused on achieving that goal. There were no threatening speeches to look to your left and to your right, in order to contemplate and tremble at your vulnerability there. I don't recall much about the economics of teaching medical students in those days, but they claimed that the tuition only paid for a small portion of our educations. This was undoubtedly true—society in general and Baylor in particular had not at that point begun shifting much of the cost of educating its future leaders and doctors to the hapless students themselves. (Nowadays medical students, including my daughter Wendy, graduate in massive debt. I should also note that the monetary environment found in the Texas Medical Center in the 1960s, awash as it seemed to be in Texas philanthropic oil-money and Houstonian civic pride and generosity, probably helped to provide some of the cushion that we no longer enjoy in our struggling medical institutions.) While at BCM, I paid a modest tuition, perhaps $3,000 per year, I was given small scholarship grants (about $700 to $900 per year, totaling about $2,500 for the four years), and I also took out small federal student loans at 4 1/4% deferred interest (also about $700 to $900 per year). I am pleased to say that I fully repaid those loans in a timely manner after I finished my residency years, and have continued to donate annually to BCM to repay the benefits and support they granted me.
The initial two years at BCM were the so-called basic science (or pre-clinical) years, whereas the third and fourth were considered the clinical years. (This distinction was not absolute when I was at Baylor, but it is much less sharply demarcated these days, as ever more effort is made to get students into earlier and more substantive contact with patients.) The first basic science year at BCM was especially well-designed to remediate the deficient educational backgrounds of even the most dyed-in-the-wool humanities majors who arrived with far less scientific preparation than I had, and by the time we had finished two years, we were reasonably well prepared in our scientific underpinnings to venture out upon the wards to deal with real patients.
I have not retained and therefore cannot bore my readers with a detailed list of my courses and grades at BCM, or exactly how we divided up courses between the first and second of the basic science years. From my first year, I have only a piece paper saying I was in the middle third of my class, which was a great relief to me. The first year included anatomy, physiology, histology (i.e., microscopic anatomy), biochemistry, and neuroanatomy (in which one is hard pressed to get ahold of anything very firm). I especially enjoyed the lovely colors and infinite variety of human tissues visible under the microscope in histology—the traditional hematoxylin and eosin stains as well as the more exotic and/or more biochemically specific stains. I was reacquainting myself with the pleasure of using a microscope that I had experienced earlier in my life. The major textbooks we used that year (only a few of which I still own) included the venerable Gray's Anatomy (27th edition, Goss), Grant's Atlas of Anatomy (5th edition), Histology (Arthur Ham, one of my favorite texts), Textbook of Medical Physiology (Guyton and Hall, now in its 10th edition), and the more compact Review of Medical Physiology (Ganang, now in its 22nd edition).
I fondly recall a few of the good teachers from those years: the gentle head of anatomy Dr. Robert Liebelt (who taught us histology), the fiery Dr. Arnold Zimmerman (a fine artist who drew gross anatomy drawings in multi-colors on the blackboard and who was known to throw his wet technicolor chalk rag at a sleeping student), the silver-tongued biochemist Dr. Harry S. Lipscomb, and many others.
Gross Anatomy: Nothing in my past education could have fully prepared me for the rigors of the gross anatomy class, the nemesis of many a beginning medical student. Gone were the abstruse worries about quantum orbitals—the task now at hand was learning how to come to grips with long afternoon labs, the corpses laid out by the dieners and awaiting our dissection, reeking of the stench of formaldehyde. We were respectful, as I recall, and did not mock the noble-minded persons who made their mortal remains available to us for such excruciatingly detailed examination, while of course we had to find ways to relieve the strain with harmlessly irreverent humor. My cadaver, which I shared with my friend William P. "Bill" Knight (also from Rice) and probably others, was a somewhat overweight female of grandmotherly age whom we called Bertha. Gross anatomy in particular presented a serious and unaccustomed intellectual hurdle to me, since at Rice I had chosen not to undergo the rigors of the comparative anatomy course that most premeds majoring in biology took. Gross anatomy entails an enormous amount of memorization of largely unrelated facts—the very antithesis of the sparsely elegant Maxwell and other equations of physics that could leave the working out of a problem merely "as an exercise left to the student". Instead, we were forced to resort to a variety of mental crutches, including bawdy mnemonics, to learn crucial details such as: (1) the bones of the wrist—"Never lower Tillie's pants, mother might come home" (the bones were the navicular, lunate, triquetrum, pisiform, greater multangular, lesser multangular, capitate, and hamate); or (2) the cranial nerves—"On Old Olympus' Towering Tops, A Finn And German Viewed Some Hops" (which translated to Olfactory, Optic, Oculomotor, Trochlear, Trigeminal, Abducens, Facial, Acoustic, Glossopharyngeal, Vagus, Spinal Accessory, and Hypoglossal nerves). This was not rocket science, but it could clearly make or break you if you could not rapidly assimilate this mountain of information. And one quickly learned that in medicine—an unbroken tradition that dates back to Hippocrates and before—the naming of objects was often arbitrary, inconsistent, multilingual, and duplicative. The names were also full of "eponyms" that, while deprecated by the academic establishment, proved in in fact to be hallowed usages that could not easily be dispensed with. (Consider, for example, the current preference for the bland and non-emotive eponymic term, "Hansen's Disease". This is preferred over the long-standing name used for the Biblical plague, "leprosy"—a disease which was related to or identical to Hansen's disease. The Biblical term was made all the more fearful through the 1959 movie Ben-Hur.) Even though the professors agreed that certain terms were out of date, the practicing physicians and working scientists made constant and unpredictable use of them. One was simply forced to learn a new and bizarre foreign language with few reliable rules. While I indeed rose to the middle of my class by the end of my first year, gross anatomy came the closest of any course to doing me in during the fall of that crucial first year.
Physiology: Physiology was probably the most enjoyable course for me during the first year, being of fundamental importance to understanding the normal functional workings of living organisms and their parts. It was the closest equivalent in medical school to the physics that I had spent so much time with in college (ignoring biophysics, a discipline not taught to med students and purporting to directly apply physical laws to biological phenomena), thus helping ease me out of the separation anxiety I felt from abandoning the college physics track. Our physiology lab afternoons were filled with stray Houston area dogs prepared by the lab assistants, usually already anesthetized in order to facilitate experiments and demonstrations of important physiological phenomena such as the functions of the heart and circulation. These dogs were "sacrificed" afterwards with lethal injections. I cannot help but marvel at the transformation that has taken place in society since then, the rise of anti-vivisection ideology and the passionate and at times even terrorist opposition to the use of animals for experimentation. At the time, it made perfect sense to me to put these animals to good use for the benefit of patients to come, and I am certain that I learned vital physiological principles as a result of this intensive lab exposure far better than more recent students who are forced to make do with more indirect or virtual forms of learning. However, my sensitivities regarding the exploitation of animals have evolved along with those of my society, and I would always want to feel that an appropriately high use were being made of any animal sacrificed in the name of medical science.
Being a cash-strapped medical student, I also began the first of many medical moonlighting jobs I held in my medical career, in this case while still a first year student. I took a crash course at the nearby Veteran's Administration Hospital, learning some of the rudiments of being an X-ray technologist. Within a few days, I took on a middle-of-the-night and weekend job taking ordinary X-rays ("plain radiographs") on emergency and sick patients, especially chests, skulls, and abdomens. This clinical clerkship, authorized by the VA Radiology Service, began April 18, 1966. I continued it until resigning just before getting married in August 1966. (We may have also called these jobs externships, though this probably misuses this term, as the clerkships were not designed as educational experiences but simply to perform needed jobs on the cheap, and we resided right on the VAH campus.) We employed technical "cheat sheets" telling us how to shoot these X-rays, but I must have been rather mediocre at this, given that good radiological technologists take two or more years to master their important skills. I did my best, but am embarrassed to think about how my inexperience might have impacted the patients—the VA must have badly needed us, and making do with inexperienced help like this is sometimes unavoidable in medicine. In any event, they put up with me (along with the many other medical students doing similar clerkships, including taking EKG's and drawing blood). Like other teams working under adverse conditions, my fellow clinical clerks working at the VA in fact developed a nice sense of camaraderie over the many months we lived and worked together there, and the food was not half bad. The job had its challenges: I recall one very large and very mean-looking male psychiatric patient whose skull I was asked to X-ray around 2 AM in the radiology department, and of course I was alone there with him. I set up the heavy lead film cassette alongside his head, but unfortunately it fell over onto his face. He glowered at me, saying,"You do that again, and I'll smash your face in." In exchange for this periodic and character-building work, I received no actual cash pay, but was granted a dorm room on the VA campus along with two "subsistence meals" each weekday and three on weekends. (In later years, I became fond of telling my own children, on certain occasions when we were grabbing a quick meal out, that I would pay only for a "subsistence meal" for them, at McDonald's for instance, and that if they wanted better, they would have to make up the difference beyond the subsistence level from their own funds.) The "quarters" that I enjoyed on the VA campus consisted of a single very plain furnished dorm room without air conditioning. I quickly arranged to buy the guts of an old air conditioner for $10. Though it lacked the normal decorative grill and facade, and one was left staring right at the whirling fan, compressor, and other working parts within, this lifesaving device would blow cold air into my dorm room and chill it down to the 50s, or so it seemed. I recall with amusement how the sweltering janitor would arrive at my room, and sit down and chat with me for a while, enjoying the cool air. We VA clinical clerks also sneaked out occasionally onto the adjacent VA hospital golf course to play a few holes, though this was officially not allowed. The patients were often to be seen on the course playing in their hospital pajamas.
Becky dropped out of membership in the Elizabeth Baldwin Literary Society at Rice in her senior year, no longer wanting to do rush week, participate in the melodrama, etc. We attended the EBLS melodrama L'il Abner on November 6, 1965 at Rice, but in general I was so busy with studies while in the first year of medical school that my participation in her Rice campus life and events fell off rapidly.
There were also only a few school-wide Baylor Med parties—mainly occasional keg parties (put on by SAMA, the Student American Medical Association), and the annual senior satirical play (which we probably attended). In my first year, I took the unusual step of joining one of the several social fraternities, Phi Chi. This was one of the few campus organizations I ever joined—I even appear in the yearbook's Phi Chi photo, and Becky and I attended some of their functions together: a wine and cheese taster on October 9, 1965, a party probably given by them on November 20, 1965, and some picnics. The purpose of these fraternities was to provide chances for social interaction, camaraderie, light-hearted fun and parties, and even some moral support for academic woes. But it became apparent to me that I just did not need or fit into the mold of traditional fraternity life, and I was becoming increasingly devoted to spending time with my future bride—thus I went inactive after my first year.
In mid-March 1966 at spring vacation, I made a driving trip with a fellow medical student, Robert P. "Bob" Witherspoon, to the Pacific coast of Mexico. We camped near Monterrey, in the mountains near Durango, and on the beach near Mazatlán. I especially enjoyed the great birdwatching on the coast: the magnificent frigatebirds wheeling overhead, and the unexpectedly graceful brown pelicans flying in balletic formation as they glided close to the undulating surface of the ocean, searching for fish.
In Becky's first semester of her senior year (fall 1965), she chose to move into the newly constructed Brown College on the Rice campus. She initially roomed alone, and had an aquarium that I gave her as well as many plants to liven up her room. By the beginning of her second semester, in January 1966, she grew tired of solitary living, and probably also wanted to experience greater freedom (for instance, from the House Mother restrictions and curfews), so she decided to move off-campus to an apartment near south Main Street. She roomed with her close friends Elizabeth, Linda, and Carolyn. It was a bustling and social place. Their focus was on completing college, preparing for future careers, and enjoying their social lives. They attached little importance to acquiring the more mundane but traditional homemaker skills such as cooking and sewing (so that it was only after we married that Becky learned much about cooking, eventually becoming a great cook). Of course, we spent a great deal of time together during this semester, and while living in the austere VA quarters, I was probably glad to have a more genteel apartment to hang out in on occasion. In the summer of 1966, she continued on in this apartment with some of these friends. She was working at Rice doing her practice teaching. It was an enrichment program set up for high school students, who wished to pay for this experience in order to get exposure on the Rice campus, while at the same time it allowed the graduating Rice education students to fulfill their state teacher's certificate requirements.
Smoking: Influenced perhaps in part by her college roommate Carol, who already smoked on arrival at college, Becky had taken up occasional smoking as a freshman in college, though never more than 2 to 3 cigarettes per day, and continued intermittently at this rate for three years. She did this at night when chatting with her friends in her dorm, apparently not on dates. I disapproved of this immediately when I got to know her, and tried to talk her out of it from time to time, initially not having enough influence to achieve this. However, when she became a senior, and we were a serious couple, we discussed it again, and she recalls my making reference to the various well-publicized reports from the surgeon general, etc. Finally, as a concession to my strongly felt belief and our developing sense of wanting to please each other on important and long-range matters including this significant health concern, she agreed in her senior year to stop smoking fully. Ironically, I toyed with non-inhalational pipe smoking in my second year of medical school (after we had married and settled in), perhaps wanting to emulate the appearance of adult sophistication and wisdom I had thought it conferred on my Rice professors, and recalling the rich aromas from childhood exposures and beyond. But I was aware of the inconsistency and inevitable hypocrisy of my actions (despite the presumed lower risk compared to inhaling cigarette smoke). Soon, I also gave up the meerschaum and briar pipes and the pleasant scents of the various pipe tobaccos—Half & Half, Sail, Turkish tobaccos, etc.—and never again dabbled in the pleasure of tobacco products, nor did Becky.
Family Events 1965 – 1966: Russ married Laura Anne Moore in July 1965. In the fall of 1965, Scott was in Robert E. Lee High School in Houston, living with my parents, and Russ had begun a year-long tour of duty serving as an MP in the US Army in Vietnam.
My uncle Russ Wait died in c. May 1966. In addition to being an engineer, he was an outstanding banjo player, having recorded some fine LPs with his Dixieland group, the Delta Kings. He loved this kind of music, and perhaps as he might have wished, he died while performing in a Dixieland group at Shakey's Pizza Parlor in Houston. Becky and I had enjoyed seeing him perform there earlier. He was one of my favorite relatives, a kind, soft-spoken, generous person, though we rarely crossed paths.
As the summer after my first year approached, my strong interest in physiology led to an offer to participate for 2 1/2 months in a Summer Research Student Fellowship as a physiology trainee in "Biomedical Electronics", funded by an $850 grant from the U.S. Public Health Service. (The USPHS was a division of the Department of Health, Education, and Welfare, or DHEW.) My project was entitled "Distortion of Bioelectric Events by Metal Microelectrodes". (I co-wrote an in-department paper entitled "Distortion of the Electromyogram by Metal Electrodes" with fellow medical student David Coyer, probably during that summer.)
I worked under Leslie A. "Les" Geddes, MD, a physiology professor with a PhD in electrical engineering and who was interested in instrumentation, and indirectly under the department chairman, Dr. Hebbel E. Hoff. These were distinguished and powerful men at BCM, respected researchers in the cardiovascular-surgery-intensive Texas Medical Center. Each summer they held a world class course in practical physiology, very much like the lab I attended as a medical student. The participants were research scientists and practicing physicians who came from all over the world. I was privileged to attend the lectures, labs, and other events of that symposium, mostly as an observer though I helped out where I could, and greatly enjoyed this summer devoted to physiology. One of the high points of this course was a field trip to Texas A&M in College Station, where we joined a research veterinarian to perform physiology demonstrations on a living anesthetized horse. (Unlike in our dog experiments, this horse was reawakened at the conclusion of the demonstrations, and not sacrificed to science.) One of the most dramatic demonstrations was the so-called Marey maneuver or Chauveau-Marey maneuver on an anesthetized horse: When the long and well-gloved arm of the demonstrator (including at one point Becky and myself) was inserted far up the horse's rectum and colon in order to compress the abdominal aorta deep within the abdomen, the blood pressure correspondingly rose from the sudden blockage of circulation, and the heart rate fell, a compensatory response called the Marey reflex or Marey's Law. (This trip reminded me of another visit to College Station. In high school, I went there for the first time with my girlfriend Jane to visit with some of her Aggie relatives, and was amazed to discover that some of them not only recalled the Civil War vividly, as if it had ended only a few days earlier, but seemed to still be fighting it.)
The participation in the electromyography research project under Dr. Geddes led eventually to my coauthorship of a published article (note 1). This summer was one of the last times I tested my wings as a laboratory-based medical researcher, in which I would be working primarily on biomedical testing apparatus. Even by then, it was becoming apparent to me—who after all did not have the electrical engineering background of Dr. Geddes and had not survived the rigors of Rice experimental physics entirely unscathed—that my focus would not lie in the impersonal electronics lab, but rather in a more traditional though high tech physician pathway centered around direct patient contact and care.
Despite my richly rewarding physiology experience that summer, I confess my attentions were not entirely focused on medicine. Becky and I had become engaged by the fall of 1965, and the last of my worthy competitors had long since fallen away. There had developed a very comfortable and natural progression of our feelings for each other by then, and it was clear we were both ready at last to make this commitment. (We were only 21 or 22 when we became engaged, which some folks now say is too young, but it sure felt right at the time.) There was no engagement ring (poor as I was), and I also did not find the opportunity to get down on bended knee to ask her for her hand—though I would have gladly done so had it been expected. I was probably unsure whether she would feel I was an adequate candidate for marriage, because of my limited economic means and other insecurities. But Becky tells me that she was the one who first brought up marriage, undoubtedly to my immense relief. When we informed her mother that we wished to marry, I learned to my chagrin that I needed to ask her father for permission. Being the nontraditional iconoclast that I was, and fearing that I might still encounter an insurmountable barrier to our union, I wondered how I might respond if he turned us down. But fortunately, he was favorably inclined to me, and readily granted his blessing, relieving my anxiety in an instant. According to Becky's calendar, we went shopping for our wedding rings on May 17, 1966.
Becky comes from a large extended family living, many of whom lived in a small town called Katy, situated about 30 miles west of downtown Houston. In the 1960s, it was still largely a rice-growing farming community, although the cancerous expansion of Houston has since tended to convert it into another exurb of that rapidly sprawling city. The Cardiff name was very prominent as one drove into town, being impressively emblazoned on several large rice dryers towering over the flat plain. Rice farming was big business in this City of Churches. Becky's father Charles I. Cardiff (1918 – 1997) was married in 1941 to Becky's mother Joyce (born in 1922). He was the eldest of four brothers (namely John, married to Betty, Tom, married to Nancy, and Hal, married to Lynn). They shared a rice farm that had been farmed before them by their father Charles C. Cardiff (c. 1878 – c. 1946) and his brother John V. Cardiff. (The latter two brothers had made their way to Texas apparently to establish a new farm that would allow them to escape a smelly pig farming business in Illinois that was run by their father, John R. Cardiff, born c. 1860.) The Cardiff family memoirs, were they ever to be written, could easily overwhelm my own long winded memoirs—and I feel I should for the most part defer to Becky to let her tell the story of her own family, and the events and persons in her life before me. However, suffice it for now to say that I was warmly and hospitably received by her parents, along with the extended Cardiff family in Katy, and was made to feel at home despite our differences in background and experiences. I enjoyed getting to know Becky's two brothers, Charles C. Cardiff, II (born 1946. married in 1970 to Linda Brown) and David. L Cardiff (born 1951, married in 1974 to Mary Beeler). Becky's father, "Mr. Cardiff"—whom I found a better name for only in 1971, "Granddaddy"—was a highly respected citizen and leader in his community. He was both a real gentleman and a devoted farmer, but he was no "gentleman farmer". Farming rice all day in the Katy summer heat was very hard work, and we could always find him out at the farm, preparing the water pumps and levees, planting the rice fields (not paddies) in the spring, assisting with fertilizing and crop dusting and irrigating, and harvesting using combines in the summer and fall. There were also some cattle to tend. He had discontinued his college education at Schreiner College in Kerrville Texas after about a year, probably because he was needed on the family farm and perhaps because farming was simply more to his immediate interest than academics. (Becky's mother attended the University of Texas and the University of Houston for about a year and a half altogether.) He was a naturally intelligent and mechanically gifted man who, especially in his later years, showed his nostalgic love for old cars (mostly Model T's), antique tractors and threshers, and other machinery and implements from the earlier days of farming. (Much of the warehouse-sized collection of antique farm equipment and vintage autos he accumulated can now be viewed at the Katy Heritage Museum.) His mother Florence I. Cardiff (1890 – 1980, called "MaMa") was one of my favorites, a very warm and generous person who always made room at Christmas and Thanksgiving for her ever-growing family gatherings. I felt gratified and warmed to find myself becoming associated with such a stable and seemingly secure extended family, contrasting it as I did with the less settled life of my own family. The Cardiff family was large enough to have a few conflicts and skeletons of its own, but all-in-all, the uniting effect of the family farm and of the beneficent matriarch, Florence, helped to hold the family together.
I have lumped mention of Becky's courses during her senior year with discussion of all her academic courses at Rice. Needless to say, she successfully survived the rigors of the Rice academic curriculum, though with a few scars from battle. Her Baccalaureate Service was June 3, 1966, and she graduated June 4, 1966 with a BA degree in biology, and with French as a minor. Both celebrations were held outdoors along the east side of Lovett hall. She was well on her way to qualifying for a teacher's certificate and a career in teaching.
 Becky with her parents at her Rice graduation June 4, 1966 |
 Rebecca August 1966 |
 Rebecca and Michael with wedding party August 30, 1966 |
 Rebecca August 30, 1966 |
The planning for our wedding was of course mostly
between Becky and her mother, and Becky became immersed during the summer in sending out
invitations; selecting her gown at a bridal shop; attending various showers and
receptions (a kitchen shower at Kaphan's, a shower at her friend Marilyn Miller's house, a
family shower at Hal and Lynn Cardiff's house, and a luncheon at the Warwick
Hotel put on by Marie Morris); and making other essential preparations for marriage. An article in The Brookshire times June 23, 1966
tells of our
engagement and included a photo of us. I was only a small cog in the
wedding machinery, but I was grateful
to be able to discuss my interest in the music to be played by the church organist, Mrs. Ruby Woods. She advised me that some of my
suggestions, such as A Mighty Fortress, would not be ideal at a wedding, but she
liked my interest in the music and we readily arrived at a good set of choices, to
include organ arrangements of the Jeremiah Clarke Prince
of Denmark's March and/or Purcell's Trumpet
Tune, probably the bridal chorus from Lohengrin, probably the Mendelssohn Wedding March, and other classical
wedding favorites.
The wedding was held August 30, 1966, four days after my physiology course came to an end, in the Katy Methodist Church, with the family's minister, Brother Leslie T. Griffin, officiating. He presented us with a booklet containing the Certificate of Marriage, along with the text to The Order for the Service of Marriage which he carefully annotated with the exact wording he inserted—where to pause for responses, etc. He read from I Corinthians 13, which celebrates benevolent or divine Love (note 10). I may not have possessed the religious convictions entirely consistent with such a Christian wedding, but I will always appreciate the opportunity to marry in a traditional, morally meaningful, and hallowed setting (and I try not to demand of myself absolute self-consistency in such matters). My best man was my brother Russ (newly returned only the previous month from his year's tour of duty in Vietnam), my groomsmen were my brother Scott and my old friend Tom Duncan, and fellow BCM medical student Rick Matsen served as an usher. (We attended Rick and Anne's wedding later in December of the same year.) The maid of honor was Marilyn Miller, and the bridesmaids were Gwen Cardiff and friend Elnora. I could still fit into the tux I had used for high school cotillions, though it was by then a little snug. We exchanged simple gold bands which we both still wear, purchased for about $30 each—I can't imagine a more perfect symbol of marriage. The church was filled with lovely candles, the scale of the wedding seemed appropriate (unlike the frequent excesses indulged in these days), the sole wedding planner was not obtrusive, and the reception was held in nearby rooms, alcohol-free as was the custom of this church. I don't remember much about the wedding ceremony, and was somewhat uncomfortable as usual to be at the center of such attention, but I was very, very pleased to be married at last to the girl—now young woman—of my dreams. I was grateful to Becky's parents for helping make possible such a lovely and deeply meaningful wedding experience.
At the risk of overdoing Platonic allusions, I'll mention that I am fond of the allegory on the origins of love attributed by Plato to Aristophanes in Symposium. He speaks, comically but with profound psychological insight, about the idea of previously united androgynous organisms that had four hands and four feet and that were split apart by a resentful Zeus. These sad but still living half-organisms fervently desire finding and reuniting with their counterparts. To me, Becky seemed just like my missing and complementary half who would make my life whole at last.
We moved into an attractively landscaped older (1930s or 1940s) apartment complex, the Parklane Apartments at 5701 Jackson #606, across Hermann Park from BCM. (Apparently these low-rise apartments have been replaced by a high-rise building called The Parklane.) We were paying $122 per month initially ($132 eventually) for a two bedroom upstairs apartment. It was a pleasant walk—when the heat allowed—through the park to my medical school about a mile away. We had been very generously treated by the extended family members and the friends of both families, and had received new furniture with which to start our married lives, including a bedroom suite that we still use, along with many other practical gifts. We had no time for a honeymoon then, and all too soon I had to begin my second year of medical school and Becky began teaching. We were poor financially, our then merged liquid assets being no more than $600, and we had few tangible assets other than our furniture and our blue and red Corvairs—thus there was no need for a prenuptial agreement! But our prospects seemed promising and we had a great life to look forward to, provided we kept working hard.
We enjoyed quiet pleasures during my medical school years, going out for barbecued chicken at a favorite joint, "Smok-a-Chik", having dinner with friends including Joe and Diana McSherry, going to the symphony on occasion, and visiting with our families. I remember the sense of domestic pride and satisfaction I experienced in making our first significant appliance purchase, a Kenmore canister vacuum cleaner. Becky took sewing lessons including dressmaking with her friend Pat, and made a few dresses at the time—her parents had given her a Singer sewing machine a few years earlier. I took only a few occasions to play tennis with friends including Rick Matsen during medical school, and exercise probably unwisely took a back seat to more pressing matters.
Movies I especially enjoyed during 1966 – 1969 included Doctor Zhivago (seen with Becky April 1966), Who's Afraid of Virginia Woolf? (1966), The Graduate (1967), and 2001: A Space Odyssey (1968). We probably watched little TV then aside from Walter Cronkite on the CBS Evening News. We took up the quiet, inexpensive, and very satisfying activity of birdwatching (which is outstanding along the Texas migratory flyways). We were helped along by a delightful and enthusiastic older English couple, "Boots" and her husband H. A. J. "Jerry" Evans, and by Becky's father, who was also quite a birder. We liked to go out to Becky's farm and other nearby farms, where huge flocks of snow and blue geese could be seen, along with lovely egrets, herons, and sandhill cranes. If you were very lucky, you might encounter the elusive pileated woodpecker—we saw and heard one only once while in Texas, in a deep woods setting on the Settegast Ranch, where we had secured permission to camp overnight c. October 1967. We joined in a few outdoor outings with classmates, such as a single-engine plane trip to Mustang Island, near Port Aransas, with the McSherrys (October 1968). We also made a pleasant canoeing trip with several couples in Louisiana on the Atchafalaya River in the heart of Cajun Country. We stayed in a rustic cabin on that lovely river, and enjoyed dining on crayfish at the nearby Cajun seafood restaurant Pat's in Henderson. The custom there was to toss the crayfish shells on the sawdust floor, making for crunchy footing. We made another canoe trip on the swollen San Jacinto River near Houston, probably in 1968, thus anticipating the craze for river canoeing later inspired by the 1972 movie Deliverance. We also ventured for the first time as a couple into the frozen north in December 1968, downhill skiing with another couple at Winter Park and Idlewild, Colorado.
In the second pre-clinical year, we applied the basic sciences that we had learned in the first year more specifically to the study of disease (as opposed to normal function), and as I recall studied pathology, pharmacology, microbiology, medicine and introductory physical diagnosis, and also received more directed exposures to the specific systems of the body and to clinical specialties such as psychiatry. The courses were becoming more and more practical and aimed specifically at the task of training real doctors in subjects they would actually need to know about to help patients, including of course the study of diseases and their effects. This period in my education more or less blurs into an unreconstructed myriad of lectures, labs, and demonstrations in the classroom and in smaller tutorials. On the basic science side of things, I was interested to see for the first time the effects of actual enzyme reactions demonstrated using living liver tissue—no longer was I merely reading about some hypothetical enzymatic reaction in a biochemistry textbook. Pathology included autopsy demonstrations—often at Ben Taub General Hospital—of victims of atherosclerosis, tumors, and infections, etc. In psychiatry lectures, the imposing Dr. Shervert Frazier would place patients before us to demonstrate their innermost psychopathology—manifestations of Huntington's Chorea, Wernicke-Korsakoff syndrome, etc.—leaving me squirming in sympathy at the discomfort the patients must have felt to be laid so bare. (He was also reputed to make medical school applicants squirm in interviews as well, for instance by asking them if they masturbated, ostensibly to test their tolerance to stress.) We learned about the workings of the kidneys, heart, skin, liver, adrenals, and other important organs. The head of ophthalmology liked to say, in this cardiovascular-disease-intensive environment, that "the heart beats that the eye may see", and I could relate to this. We were exposed to experts from virtually all areas of clinical medicine. One slender cardiologist, Dr. Lawrence Lamb as I recall, was an early adopter of vigorous aerobic exercise based on its health benefits, one of the first persons holding this belief to which I was exposed. BCM heavily emphasized research, so the physicians and scientists that spoke to us were often researchers who were well-known in their fields—it was an inspiring experience indeed.
Some of the major textbooks I read included Pathology (by Robbins, currently termed Pathologic Basis of Disease by Robbins & Cotran and in its 7th edition in 2011), and Harrison's Principles of Internal Medicine (in its 17th edition in 2011).
Whatever the actual sequence and organization of our basic sciences course work in those first two years, and this is an area undergoing constant evolution in all medical schools, I felt that the quality of the teaching and the effort that went into preparing this pre-clinical educational experience could not have been better. I am truly grateful for the outstanding education that I received at Baylor Medical School, especially during the basic science years, even if I did not always feel I had sufficient bio-horsepower to rise fully to the demands made on us.
Being surrounded by such excellence and academic ferment was always somewhat intimidating—I wondered, where in this system would I be able to fit in?—but such tension and discomfort is inevitable and unavoidable in the world of medicine. (Medical education even for established physicians continues far past medical school—so-called Continuing Medical Education or CME. This tension arises because of the constant changes in factual knowledge and concepts resulting from research in the supporting technologies, or from evolution of societal attitudes and values, etc.)
As each expert came through to give a lecture, the medical student was constantly trying on new hats for fit, asking, "Is this the one I will be able to wear for my career?" Of course, there were some students who already seemed to know exactly how they wanted to fit into medicine—being a country family doctor, or a surgeon, or a psychiatrist, for example. For most of us, however, the possibilities to consider were almost limitless, and we were exploring what directions to go in: Research versus clinical practice; academic environment versus private practice; focus on lucrative specialties versus less well compensated humanitarian service; treating the wealthy versus the underprivileged; confining one's work to a limited and local setting (big fish in a small pond approach) versus striding forth onto the international stage (small fish in a much larger pond), etc. Fortunately, medicine allows its members to change their minds about career choices, and to try a new specialty or practice setting even after initially settling down into a particular role.
My background in physics, the three summers of experiences at M. D. Anderson Hospital, and my general interest in physical science and complex technologies made radiology and nuclear medicine seem to be good possibilities for my choice of specialty. Dr. John A. Burdine, Jr., who was the head of nuclear medicine and a good salesman for that field while I was at Baylor, got me interested in nuclear medicine technologies that were just then coming into use, such as the 111-Indium radioisotope generator (about which I wrote an in-department paper). I was also exposed to good radiology lectures by Dr. Magdalena "Pogo" Pogonowska, by the medical physicist Stewart C. Bushong, Sc.D., and by others in radiology, and I was favorably predisposed to some type of radiology career by the end of my second year. (See here for why I finally chose radiology.)
Medical Journals and Articles Collection: I began a lifelong subscription to the excellent New England Journal of Medicine in my first year of medical school, and also tried out subscriptions while in medical school to Science, the Annals of Internal Medicine, and The Medical Letter. I continued to enjoy Scientific American, which I have used since c. 1958 to broaden my science background beyond my immediate professional needs.
Faced with a burgeoning mass of medical information on paper, I also began by my second year of medical school to develop an elaborate system of filing reprints and medical articles. A large and inspiring collection was proudly maintained by my respected medical school mentor, the internist Dr. Herbert Fred. I designed my filing system initially around a numerically-coded system advocated by the hematologist, educator, and classic hematology textbook author, Dr. Maxwell Wintrobe. I continued to expand this system throughout my active medical career as my collection grew. By the time I retired, I had 24 file cabinet drawers packed with useful medical articles, not limited just to my specialty but including key articles in many medical fields, cataloged by my own alphanumeric filing system that that had served me extremely well. Of course, medical information retrieval in the computer and Internet era has radically evolved and has become much more diverse in its possibilities. But while working in the trenches in image-intensive radiology, I found there was no substitute for being able to place my hands on a key recent article when called upon to render an important opinion on short notice. If you are pursuing a medical career, you should organize your paper or electronic articles early and with a system that can grow with your collection!
My Performance: I seemed to be doing OK academically, falling in the upper third of my class and making the Dean's Honor List during my second year.
The Virtue of Medicine: I took great satisfaction in knowing that medicine in its myriad forms was almost always intrinsically useful and good. Provided I made reasonable and ethical choices, I would never have to worry about whether what I was doing was actually beneficial to humankind. Given my tendency to agonize about almost any such moral question, this was a great relief.
Moonlighting: As a second year student, I was continuing to find moonlighting where possible, earning $100 with Ben Taub Hospital doing some clerkship task, and taking on the night medical librarian job at the Methodist Hospital (which paid me $334 in 1967, and gave me mostly a quiet, cool, and pleasant place to study).
During September through December 1966, Becky taught five classes per day in Biology and French in an intern-like status at low pay at Memorial High School in the Spring Branch Independent School District. In January, she was hired there in a full-time regular position, still teaching biology and French. She earned about $300 per month gross as an intern. Becky's diligent work as a teacher was certainly our main means of support—she earned about $5,300 gross in 1967, which included teaching summer school all three months of 1967 plus some tutoring. We kept our expenses low, and tried to live within our means.
Although she may have come from a comfortable and somewhat privileged background, she has always been a hard worker and did all she could to do her part for our mutual support. She applied herself to the task of teaching with her usual high striving for excellence—I believe she did quite well at teaching and she earned much praise from her superiors. This teaching role, lasting as it did only three years, was one of the professional highlights in her career. (She took on a new career as a diagnostic sonographer much later in life.) Classroom discipline could be a problem then just as now, but the principals supported the teachers much better than now, and Becky knew she could send a problem kid who was getting out of hand to the office rather than being forced to contend on her own with rebellion and threats in the classroom. One problem student stole her gradebook, tossing it in a ditch, and eventually came to class clutching a menacing crowbar. (I am reminded with some disgust that when Becky explored the possibility of teaching in the Seattle public school system in the 1990s, she was informed that teachers should for the most part handle their own discipline problems in the classroom, and not expect to send problem kids to the office, and that ex-policemen and ex-firefighters best fit the model of what was needed in teachers.) A favorite mentor in her teaching life was Mrs. Jess Anthony, a lively older biology teacher and a real role model for Becky (and for me as well). She initially had served as an adviser for Becky in the summer school enrichment program that was the first part of the practice teaching experience for the education graduates. We enjoyed making several biology class field trips to the Big Thicket 50 to 75 miles away, a woodsy wilderness (now a National Preserve), where Jess helped us explore the biological wonders, including carnivorous pitcher plants, a wide diversity of trees, woodland birds, and a nice assortment of spiders. By going along on these school outings, I got to experience vicariously what an enjoyable career in teaching biology might have been like, had I not elected to continue with medicine.
Division of Labor and Her Career Aspirations: We had no sense in those days that Becky was somehow sacrificing her own career potential merely to play a supportive role nurturing and backing up my own ambitions. I have never doubted that, if Becky had encountered different circumstances and needs in her life, she had what it took to continue on to become a fine physician or research scientist. While I passionately celebrate the greater freedoms and career opportunities that women now enjoy partly as a result of the feminist movement, we have both seen many professional couples in which the division of labor (including child-tending duties) is awkwardly worked out, and becomes a source of constant tension in leading to marital conflict and in some cases to divorce. Fortunately, the division of labor in our early marriage years and beyond happened almost effortlessly, since we both were trying our very best to make it all work smoothly, and neither of us had any perception of inequitable exploitation, unfair sacrificing for the other, etc.
Nature Interests: We steadily built on our mutual and growing interest in the natural living world during those early married years and beyond, acquiring a number of field guides and other books on plants and animals which we took on our outings, visiting the Aransas Wildlife Refuge, Big Bend NP (with her family), and Huntsville State Park or nearby Sam Houston National Forest (July 1967). Becky continued to expand on her love for plants by gradually filling our apartment with a variety of beautiful interior house plants: Dieffenbachia, Philodendron including Monstera deliciosa, Dracaena, Kalanchoe (the "mother of thousands/millions"), Rubber Plant (Ficus elastica), Ti Plant (Cordyline terminalis), Schefflera (Brassaia actinophylla), Jade Plant, various ivies, etc. She grew a Spider Plant (Chlorophytum comosum)—and still propagates it to this day—that derived from the original cutting found in her bride's bouquet that she tossed at the wedding. (My step-grandmother Edith Wait made starts from it, raised these in her hydroponics greenhouse, and later gave us our own spider plant start arising from the bouquet.) Becky also kept up the aquarium I had given her for her birthday in her senior year, and we enjoyed watching the colorful neon tetras, black mollies, swordtails, angelfish, and loach. (We donated this aquarium to the Memorial High school, at which she taught, when we moved to Colorado.) We gradually also accumulated a fine seashell collection that we started while I was a junior in college, mostly through purchasing. But I also gathered some with beach collecting, especially in Galveston after a major storm, in Fort Lauderdale in 1965, and on a trip I made to Mazatlán in 1966. We had a good assortment of augers, conchs, cones, cowries, murexes, olives, periwinkles, tulips, wentletraps, whelks, etc. One of our prize specimens was a rare Strombus taurus (bull conch) given to me by a health physicist at M. D. Anderson, who acquired it while monitoring radiation dosages and side effects arising in the local islanders from the hydrogen bomb testing in the Marshall Islands.
Guinea Pigs as Pets: The first pet we had as a married couple was a medium-brown guinea pig which I rescued from one of the Baylor Med labs after its experimental role had concluded. We named it "Nemesis", perhaps because the lab would otherwise have been its nemesis. Nemesis developed a Vitamin C deficiency, as the inadvertent result of an improper diet, and tragically died despite a desperate trip we made to a vet at Baylor Med when we finally realized the gravity of the situation. We had two more guinea pigs from 1966 to 1970. "Proteus" was a multi-colored pet who liked to be cuddled, and would lay across our lap, but had an unnerving tendency to suddenly jump up as if having a mass spasm when scurrying along the rug. We moved our third guinea pig, "Piggy", to Colorado where I interned. It had beautiful chocolate brown fur and was very also comfortable being held and cuddled on our laps. Becky enjoyed talking to these pigs in a high-pitched voice, which she subsequently imitated in talking to wild pikas and marmots on mountain hikes to great effect.
Mexico Trip 1966: After the enjoyable physiology summer of 1966 (discussed above), I never again had a free summer off in which to consider an extensive vacation until I retired. From this point on in my medical career, medical education and work became year-round tasks to pursue, with vacations scheduled and interspersed according to the prevailing rules. However, we did take a nice driving trip to Mexico City during Christmas 1967, a trip we regarded as a sort of delayed honeymoon. We toured the recently opened and impressive National Anthropological Museum, learned what real Mexican food tastes like, toured the pre-Aztec ruins and pyramids at Teotihuacán, and enjoyed learning a little more about other attractions that Mexico offers. (It is remarkable that we Americans tend to know so little about this beautiful country on our southern border.) We sampled the Mexican delicacy that my father loved, cabrito (roasted kid goat), in a small Saltillo cafe now called El Meson del Principal (still there in 2011, though Coahuila is now a risky state to visit). While we were dining there, a man brought two bleating kids through the front door and right past us—ideally, cabrito is made from suckling kids at only thirty to forty days of age—and before we left, these kids were roasting on a spit in the front window.
Family Events 1966 – 1967: While I mostly kept my nose to the grindstone in medical school, events in the outside world were swirling ever more out of control. My mother filed for divorce in spring 1967, based especially on a need for greater financial independence. The divorce was finalized in December 1967 and was a devastating development for my father but in all likelihood the right thing for her to do (see parents). I grieved for what seemed to be this final symbolic disintegration of my original family, and its impact especially on my father. (However, I was grateful that my parents, despite the divorce, went on to maintain generally good relations and would, for instance, come to visit us and celebrate holidays together.)
Outside Events and Politics 1966 – 1967: On the larger world stage, President Lyndon B. Johnson (1963 – 1969) was re-elected to his first full term in 1964, promoted his Great Society, but also massively escalated our involvement in Vietnam. (As I recall, he was the first presidential candidate I could and did vote for.) The war was not going well, and by spring 1967, massive protests were taking place. Accompanying the much needed cultural revolution epitomized by the civil rights movement, the many violent domestic tragedies of the latter half of the 1960s were playing out, including the assassinations of the Rev. Martin Luther King in April 1968 and soon thereafter Robert Kennedy, the race riots of Watts (1965) and Detroit and Newark (1967), and other drastic societal upheavals. I grieved for my country and its suffering. Even now, I feel no sense of nostalgia for the 1960s: not for the Summer of Love of 1967; not for the breakdown of traditional authority and trust in government; not for the pervasive and destructive infusion of illegal drugs into our culture; not for the shameful Nixon years; and certainly not for the wrenching violence and chaos that almost tore our beloved country apart. (I voted for Hubert H. Humphrey in 1968, but sadly we elected instead President Richard M. Nixon, 1969 – 1974.) I ask myself, should I have been more overtly activist in the 1960s, more involved in demonstrations and expressing solidarity with the many swirling, confusing, and conflicting movements? I hope that history will judge me benignly for simply staying focused on the task of becoming a physician, as this role, for myself at least, surely had greater if quieter worth to society.
The Draft and Alternatives to Military Service: I had a student Selective Service draft deferment in medical school, but
was well aware that military service and particularly serving in the Vietnam
War were looming as ominous possibilities in my future. (Of
course, some lucky persons like my friend Bill Warren ended up serving in Europe for
their military service in the Army.) The military options that I believed I had
were as follows:
• Enter military service immediately after internship;
• Get a Berry Plan
deferment to complete my residency and then enter the military (in either case
hoping to snag a European assignment, which however was never guaranteed); or
• Ignore the entire situation and hope I was not drafted.
Interestingly,
I note on the web site of the Selective
Service System that according to the outcome of the lottery drawing of
December 1969, persons with my birth date and born in 1944 received a lottery
number well above the cutoff number of 195, above which no one was drafted—but
I was unaware of this at the time.
I
dreaded the possibility of military service, not wanting to abandon entirely my
patriotic duty (though many did, fleeing to Canada or just disappearing), but
nevertheless feeling that I was not cut out for fighting a war and
wondering if I might fail in the line of duty if forced to face such a difficult
challenge. Fortunately, my country provided me with an honorable
alternative for meeting my military obligation, namely serving as a commissioned officer in the United States Public Health
Service (USPHS). The potentially available options for a physician in the USPHS and
related agencies included:
• Practice in a prison;
• Practice in the
Indian Health Service (IHS) on an Indian reservation in South
Dakota or the desert southwest, etc.;
• Practice in the Indian Health Service in Alaska;
• Do medical research at the Centers for Disease Control and Prevention; or
• Do
medical research at the National Institutes
of Health (as did some of my distinguished medical student colleagues,
including Frederick A. "Rick" Matsen III)
Although the
research positions would probably be more prestigious and career-enhancing, I
had no clear orientation toward research, and had no guarantee of securing one
of these even if I were strongly interested. Moreover, the possibility of
practicing in Alaska in the IHS was just too intriguing, and this was my first
choice out of the several possibilities.
The USPHS and the Indian Health Service in Alaska: What attracted me and us to Alaska in particular? I somehow had become convinced very early in medical school that we might want to try the larger frontier and wilderness of Alaska. Alaska had become a state when President Eisenhower signed the official declaration into law January 3, 1959. The state had been celebrated in the silly 1960 movie North to Alaska (starring John Wayne, Stewart Granger, Capucine, and Ernie Kovacs), and came to greater and more serious public attention after the massively destructive Good Friday earthquake of 1964. There was also a rising societal consciousness regarding the tragic plight and mishandling of native Americans that came to the fore during the civil rights era of the 1960s and 1970s, as reflected in such books as Dee Brown's 1970 Bury My Heart at Wounded Knee and Josephy's 1969 The Indian Heritage of America. It seemed more and more logical that I might combine my military requirement with my own nascent but developing interest in doing something useful for disadvantaged native Americans, and to see some of the great state of Alaska in the process. This felicitous convergence of multiple disparate factors compelled me to seek Alaskan opportunities in the USPHS / IHS, beginning probably as early as my first year of medical school. I managed to find a contact, as I recall Dr. William Spencer (head of Baylor's Department of Rehabilitation), who knew Dr. Martha Wilson (the Service Unit Director for the Anchorage Service Unit of the IHS). Dr. Spencer put in a good word for me, unlikely as this tenuous connection from 4,000 miles away might have been, and I continued to express great interest over the intervening years of medical school in serving in Alaska in the IHS. Although the orders for this assignment were to be issued several years in the future, this early preparation illustrates how, when operating at my best, I have tended to anticipate important needs long in advance, and have left as little as possible to chance. (The flip side of my tendency for great preparedness is the label that my daughter Wendy came to jokingly apply to me, that I was a "World-Class Master of Worst-Case Scenarios". Ironically, a truly worst-case scenario came to pass when chronic illness ended my medical career years later.)
Health: My health was good in medical school, as before. During our course on physical examination, my mentor noted that in addition to having a deviated nasal septum, I also had reflexes that were so brisk as to be "nearly pathological"—we got a good laugh out of this, as it seemed to confirm my general impression that I was a little overly endowed with nerve endings.
Reactive (Postprandial) Hypoglycemia: A research physician, Dr. Harold L. Dobson, who was interested in insulin and glucose metabolism, was delighted to explore my long-standing complaints which had been attributed to reactive (postprandial) hypoglycemia. I experienced temporary onset of adrenalin-like symptoms including sweating, tremor, rapid heart rate, and other sympathetic autonomic symptoms, mild cognitive clouding, transient weakness, and eventual headache—all arising several hours after ingestion of a substantial sugar load and rapidly relieved by ingesting a meal or additional sugar. The oral glucose tolerance test (GTT) that he administered in March 1967 and carried out only to 3 hours, showed the glucose level falling only to a normal value of 80 at 3 hours, and I did not experience any hypoglycemic-like symptoms during this test. Thus, this single test did not confirm hypoglycemia under the conditions employed. Negative, poorly reproducible, or non-correlating GTT outcomes are often found in patients studied for reactive hypoglycemia, and this diagnosis and the use of the GTT to diagnose it eventually fell out of favor. But Dr. Dobson did state that the ingested glucose triggered a prolonged and excessive secretion of insulin in me (I do not know the actual test values). Delayed falloff of insulin as glucose falls might be associated with eventual hypoglycemia, because insulin drives glucose out of the bloodstream. More prolonged testing to 5 or 6 hours was advocated by some researchers, and might have been helpful in evaluating my history, or alternatively glucose testing on blood drawn at the time of onset of hypoglycemia-like symptoms, but neither has not been done. Despite the inconclusive lab results, I long ago learned that I could largely prevent the distressing symptoms by eliminating sugar at breakfast, limiting sugar at lunch and between meals, and shifting to a diet higher in protein and fat. This diet was optimized to retard gastric emptying and to flatten out the glucose peak resulting from meals having a high "glycemic load", such as had been hypothesized to trigger excess insulin secretion and subsequent reactive hypoglycemia. I wondered if there might be a relationship between my still presumed mild disorder of glucose metabolism and the diabetes mellitus found in both of my grandmothers (not to mention the presence of symptoms also suggesting reactive hypoglycemia in at least two close blood relatives). In any event, I have continued to regard this symptom as reactive hypoglycemia, and continue to control my diet to prevent the syndrome, and have never had any serious problems from it.
I have gone into substantial details about this syndrome, not only because of its intrinsic medical interest and controversy, but because it was the first encounter I had with a very real physical symptom complex which was not conclusively verifiable at least by a single, though probably suboptimal, laboratory test. (It would not be the last—see CFS.) Because the testing was inconclusive, was this symptom complex perhaps a form of psychoneurosis in an anxious and overstressed medical student? Though I do not claim any expertise in insulin or glucose metabolism, a psychiatric explanation such as psychoneurosis or somatization would be untenable from my perspective, especially because the symptoms—which dated back to junior high school days, long before I knew any medicine—are so readily relieved by sugar or a meal.
Migraine: I did not seek any laboratory confirmation regarding the other paroxysmal syndrome that I have long experienced, namely classic scotomatous migraine headaches ("migraine with aura"). My history, if it was to be believed—of recurring and predominantly one-sided headaches and mild nausea which followed a visual aura called a scintillating scotoma—was clearly diagnostic by history alone and without further testing. The headaches and sick feeling that I developed with migraine were tolerable, lasted 12 – 48 hours, and never caused me to lose work. However, the aura could definitely interfere with tasks requiring clear vision such as driving or test taking (and as mentioned, I would never have considered trying to pilot an airplane).
Thank heavens that no disability payments or other "secondary gains" depended on objective verification of either of these diagnoses (migraine or reactive hypoglycemia). From my point of view, these diagnoses were useful and reassuring clarifications regarding annoying and at times distressing symptoms that I had experienced all my adult life. If I were ever required to actually prove that I have either of these syndromes, I quite possibly would not be able do so, and this gives me greater empathy for patients with similarly elusive physical complaints.
The clinical years of medical school—that is, the third and fourth years—presented a new set of challenges (and numerous alternatives to the career I was beginning to contemplate in radiology). The focus was shifting to participating on clinical services, starting for me with the internal medicine ward at Ben Taub General Hospital. Although we continued to have didactic lectures, the emphasis was by then more on working with house staff as they took care of patients, learning from their successes and mistakes.
Internal Medicine: I learned a lot about practical medicine, having patients with disorders ranging from diabetes and dissecting aortic aneurysm to Munchausen Syndrome. My chief of medicine on the inpatient internal medicine service, Dr. Herbert L. "Herb" Fred, was one of the real characters from my medical education. He was an inspiring person whose aphorisms have stuck with me these many years (though I can quote him only in paraphrase). Although he seemed at the time almost indifferent to therapy, he was a master diagnostician, and approached the quest for an elusive diagnosis like Teddy Roosevelt hunting for big game. He was fond of hyperbole and of mocking the surgeons and orthopedists for their presumed lack of careful thought. He loved to disparage what he regarded as loose terminology, such as "stroke", and muddled thinking such as the phrase he detested, "to cover [a patient] with antibiotics" (as if antibiotics were some kind of blanket). He would disparage mythical surgeons with no intellectual curiosity who, when presented with a patient with a fish head growing out of his chest, would simply write in the chart: "Patient with fish head growing from chest, fish head removed, discharged without complications." He loved to claim that the need by medical students for sleep had never been established. (However, since then this need has been conclusively established!) He would say, of pompous physicians who boasted of and relied on their years of experience, that they instead "had only one year of experience and 30 years of repeating the same mistakes over and over again". He would relentlessly grill us medical students even after we had been up all night, but would reward with praise those of us who had taken the time to show some motivation to learn something crucial or track down important lab values during the night. The most important lesson he taught us, as far as I was concerned, was that medicine is never static but is constantly changing, that old and time-honored adages and rules of thumb can quickly become obsolete and must always be questioned, and that there is no place in medicine for comfortable complacency. I supplemented my education through patients by reading much of Harrison's Principles of Internal Medicine during my medicine rotations.
Neurology: Dr. Benjamin "Ben" Cooper was a lively exemplar of neurology, a witty man and fine teacher who as I recall came from South Africa but loved to boast (with a hint of mockery) of his "expensive classical education" gained in the United Kingdom. He was a lot of fun to visit in his clinic, and a constant goad to students struggling to learn some of the arcane aspects of neurology.
Psychiatry: I recall a moving experience in psychiatric clinic. I cared for an attractive but deeply depressed patient, and was gratified that she responded over a period of several weeks to my sympathetic care and to tricyclic antidepressant medication (the use of which came into common practice only in the 1960s). I found psychiatry too disturbing to choose as my specialty though: the human suffering was impossibly deep and triggered my own unresolved painful feelings; its scientific foundations were shaky and unpersuasive; and the field seemed to lack adequate tools to deal effectively with the problems encountered. (I had read by that point a number of Freud's writings, including The Interpretation of Dreams, Wit and Its Relation to the Unconscious, History of the Psychoanalytic Movement, Psychopathology of Everyday Life, etc., and was intrigued but put off by his highly literate but at times seemingly unscientific style. Subsequently, indeed, the scientific validity of his writings came into serious question.)
Pediatrics: Pediatrics presented yet another type of personal challenge. On the one hand, the kids were really cute and endearing, and provided me one of my first opportunities to work closely with children, complete with head lice, runny noses, and rashes. But the suffering of really sick children such as presented at Texas Children’s Hospital could be terribly difficult to confront, unfair beyond anything encountered in the adult world, and I ultimately concluded I was not really suited to deal medically with sick children on a regular basis. Thus I chose adult internal medicine for my internship, and ultimately a radiology career that rarely involved diagnosing or treating children. Our textbook was Nelson Textbook of Pediatrics (currently in its 18th edition).
Obstetrics and Gynecology: This service presented challenges of even greater physical endurance. The Ob-Gyn service I rotated onto was at an aging county hospital, Jefferson Davis Hospital (first established and unwisely so named in 1924, torn down in 1999). The charity obstetrical patients converged there for delivery, and during my rotation of six weeks or so, I actually delivered 66 babies, using low forceps, placing pudendal blocks, doing episiotomies, etc. It was a concentrated and hands-on OB experience like few medical students would have today, and I learned many practical if imperfect skills that I later applied during my general medical officer days in Alaska. This was not very cerebral work, and though it made a great impact on me as representing the coming to fruition of human reproduction, I concluded I was definitely not cut out for a career in obstetrics. I also had a good exposure to the inpatient surgical practice of gynecology, and probably limited exposure to outpatient gynecology. The textbook, which I read cover to cover, was Williams Obstetrics (now in its 23rd edition).
Surgery: Surely my greatest challenge during the two clinical years was surgery (and the associated surgical emergency department rotations). I was not by temperament well suited for this work—there really is a surgical personality type and I just did not have it. It was arduous, stressful, physically demanding, relentless, confining, irritating, at times exploitative of the medical students, and yet urgently vital for the patients. The patients at Ben Taub General Hospital especially were often victims of acute trauma (and were sometimes said to be members of the so-called "Saturday Night Knife and Gun Club"), requiring emergency surgery for wounds sustained in war-like conditions. (In fact, surgeons who trained in that program were said to be well equipped to move on to wartime service in Vietnam.) I encountered some of the least intellectual and most macho physicians and house staff on this rotation, and felt the least comfortable while on it. As with my failed sleep experiment in college, I was again coming up against personal limitations that simply could not be readily overcome. I experienced for the first time a kind of claustrophobia from being trapped for hours in the OR, enshrouded in hot surgical garb and the stifling mask, uncomfortable from sleep deprivation, fatigue, hunger and at times hypoglycemia, thirst, and deprivation of freedom—this discomfort for a while even seemed to threaten my ability to fulfill all the demands of the rotation. Would I become like Conrad's Lord Jim, who failed the test of the man when under duress, and lived out his life with guilt and shame? (Fortunately, medicine in fact provides an infinitely more graduated spectrum of heroic possibilities from which its practitioners may choose an appropriate level of expression—the Conradian black-or-white code of honor is cruel, severe, and unnecessarily rigid.) For the first time in medicine, I began to encounter some surgical house staff who, perhaps understandably, did not seem to enjoy what they were doing, and who seemed to take out some of their frustrations and hostility on me. Unhappy with my assignment, counsel was sought, a revision was made, and I soon found myself at St. Luke's Hospital working equally long hours in the OR but under a kinder surgeon with whom I could more easily work. He was an upstanding Christian man, and I recall his indignation at the immorality of the then current 1967 movie The Graduate. I also rotated onto cardiovascular surgery for a while, squeezed in at the rear of the OR behind the large team of attendings, fellows, house staff, and visiting surgeons who had come to see the great Dr. Denton Cooley operate. (He implanted the first completely artificial heart in a human in 1969.) There were some good war stories and jokes to go with the massive egos of Drs. Cooley and DeBakey (such as Cooley's purported advice to his more seriously ill patients, "don't buy any long playing records"). Overall, surgery was not a good experience, and I generally felt I could not escape that environment fast enough.
Academic Performance: Although I did not always feel entirely well suited for some of the clinical services I was exposed to, I again did well academically in my third year, falling in the upper third of my class and making the Dean's Honor List. One simple but nevertheless somewhat unusual practice I adopted contributed to my relative success: For each service I was on, I acquired a definitive textbook on the subject and read it cover to cover, in order to assimilate the widest possible knowledge from that field. It surprised me to see how few of my fellow students paid much attention to reading textbooks once the blood-and-guts clinical rotations had begun. Of course, there were times when my approach to learning medicine was just too bookish and not sufficiently interpersonal, compared to some of my more politically adept or personable colleagues.
Handling of Indigent Patients: I had the sense on my rotations in the charity hospitals, Ben Taub and Jeff Davis, that the indigent and mostly minority patients did not always receive the same level of care or consideration that the more well-heeled patients received at the Methodist Hospital or the other private hospitals. There was sometimes a suggestion of exploitation in how these patients were handled—they seemed to be serving a role as teaching cases or research subjects that they did not voluntarily choose. Fortunately, the whole field of medical ethics has evolved markedly since I was a medical student, the bar has been raised considerably higher on what is considered appropriate patient handling, race-related inequities in medicine are much more openly discussed and challenged, informed consent is now mandatory both in principle and in practice, and there is a much greater emphasis on the rights, the privacy, and the dignity of every patient.
Income: Becky continued to keep us afloat financially, earning a gross of about $6,200 for 1968 from her teaching (a monthly gross of about $480/mo for classroom teaching during the regular school year). My medical school moonlighting had nearly come to an end due to the heavy demands of the clinical rotations—I earned only $79 in 1968 from Methodist Hospital library work and $110 from St. Luke's cardiology in May 1969.
Attracted to learning more in and about the great cultural mecca, we drove my blue Corvair in the summer of 1968 to New York City, where I had lined up a clinical externship in inpatient neurology at the Columbia Presbyterian Neurological Institute (aided by a PHS externship grant totaling about $800). The former chairman of the neurology department there, Dr. H. Houston Merritt, was the author of the well-known Merritt's Textbook of Neurology (a text that I read much of, first published in 1955 and in 2011 in its 12th edition). There was an exceptionally able team of attending physicians, house staff, and students. One of my neurology residents was Dr. Bertel Bruun, who besides his substantial medical talents was a noted ornithologist. He had coauthored the most popular field guide to bird-watching, Birds of North America, as well as several other bird books. Becky and I enjoyed accompanying him on a trip or two into the field to view birds, including one at the Jamaica Wildlife Refuge near Idlewild (now Kennedy) Airport on Long Island. I was trying on the neurological hat for size that summer, but eventually concluded that neurology was excessively cerebral and did not quite meet my needs (though I received a high commendation from Dr. Richard Masland, the chairman at the time).
Becky's Summer Job: During that same summer, Becky participated in a research project with Columbia University School of Public Health and Administrative Medicine, in which she earned $424 gross (a job again apparently arranged through the networking connections of the Houston epidemiologist Dr. Eleanor McDonald). This involved a survey on abortion attitudes in the New York City area, and she enjoyed getting to know some of the real Jewish mothers who worked on the project and looked after her attentively and maternally.
Life in New York City: The summer in Manhattan was my first in-depth exposure to a truly international environment, with a rich panoply of ethnicities to enjoy. As I recall it was the first real opportunity I had to mingle with blacks who were fully integrated into the social setting, such as at parties and gatherings given by medical students and house staff. By this time, at least in New York City, the "black is beautiful" movement was in full swing, afros were sported in great numbers, and blacks were emerging from the underclass to assert and assume their well-deserved place in mainstream society. We sublet an apartment in an aging but once elegant building at 900 Riverside Drive, paying $110 per month. We were glad to have an assortment of security bolts and bars on the door there, and we were learning more in general about coping with the challenges of big city life. These included broken elevators, garbage piling up on the sidewalks during a strike, stifling heat as the summer progressed (inhibiting any desire to cook), and getting around without a car. It was a good summer to explore the riches of New York City (see also music), the museums, the ethnic people and foods (including bagels, rollmops, and other Kosher deli foods), plays such as O'Neill's Moon for the Misbegotten, The Prime of Miss Jean Brodie (based on Muriel Spark's novel of the same name), Stoppard's Rosencrantz and Guildenstern are Dead, musicals including Man of La Mancha and Hair, and several of the Joseph Papp Shakespeare productions in Central Park.
Touring in the East: We also used this trip to become more acquainted with other parts of the East, including Cape Cod, Boston and Concord, New Hampshire and Vermont, Montreal and Quebec, New Brunswick, Nova Scotia, Maine, and Pennsylvania. I especially enjoyed visiting with and getting to know better the family of uncle Bill and Dorothy McGoodwin, who lived in Lexington Kentucky. We got to meet my cousins Patrick L. "Scooter" and Robert A. "Robbie" McGoodwin for the first time. (My other Kentucky cousins, William S. "Bubby" and Thomas H. McGoodwin were not in town at the time.) We also visited in Lafayette Louisiana with my uncle Jack Wait (1912 – 2001) and aunt Aline (1915 – 2000). Regretfully, I have not found enough opportunities to keep up well with most of my other far-flung cousins and the other descendants of my father's brother or of my mother's siblings. This was a major car camping trip for us, a good opportunity to experience more of the outdoors including some fine birdwatching, and one of the longest driving trips we have made at about 7,500 miles.
My father found his newly divorced status extremely distressing. My mother moved back to San Antonio, beginning in the fall of 1968, and lived alone until she and my father remarried in late 1979. Russ resumed college work at the University of Texas in about this year, working on a graduate degree in the department of Anthropology. Russ and wife Laura Anne divorced in 1969. Scott earned his GED, attended classes initially at San Jacinto Community College, subsequently moved to San Antonio, and attended classes at San Antonio College (formerly called San Antonio Junior College).
Clinical Courses 1968 – 1969: During my final year of medical school, I continued the clinical rotations described above. One rotation gave me an exposure to the decidedly less high-tech world of public health, in which dedicated nurses and other professionals fanned out in the greater Houston area to deliver care to the more needy of its inhabitants. I also enjoyed rotating through or otherwise being exposed to some of the specialties including hematology (mentored by the excellent Dr. Edward Lynch), ENT, anesthesiology, ophthalmology, and radiology.
Alpha Omega Alpha: I was elected in September 1968 to permanent membership in the Alpha Omega Alpha Honor Medical Society, an honor that I treasure from my medical school days. This membership includes a subscription to The Pharos, a thoughtful and scholarly publication with good movie reviews written from a physician's point of view.
Seeking and Preparing for Internship: During this final year, I applied for adult internal medicine internships in Denver, Portland Oregon, and probably Seattle, as well as in the Baylor Medical School system in Houston. These internships were free-standing one year programs at the time, though now internships are fully integrated into residencies. (When I trained, it had not been too many years since the time when most physicians simply went from their internship year directly into medical practice.) The trip to Portland to interview at the University of Oregon Medical Center (now Oregon Health & Science University) was my first exposure to the glories of the Pacific Northwest. I stayed with our friends John and Pat Burkhardt. (John was a BCM student one year ahead of me, she was a teaching colleague of Becky.) They introduced me to freshly caught salmon, Cannon Beach, Multnomah Falls, and Mt. Hood—a truly spectacular region of the country which would soon lure us back. Through the National Intern Matching Program, I was accepted in March 1969 into my first choice, the "straight medicine" (i.e., internal medicine) internship at the University of Colorado Medical Center in Denver, to start June 23, 1969. I bought a new 10-speed bike for $62, anticipating that I would be able to ride it to work in Denver where we would have only one car. Becky's parents generously bought us a new car, probably as a graduation present for me, a 1969 Chevrolet Chevelle Malibu coupe, for which we traded in her red Corvair, and soon we also sold off my trusty blue Corvair as well. The two Corvairs had served us well and kept us safe enough, despite the bad rap from Ralph Nader's Unsafe at Any Speed. (However, one day we both experienced severe carbon monoxide-induced headaches from her Corvair's leaking exhaust pipe—the fumes were somehow sucked into the car through the window well while the air conditioner was running during an extended outing.)
Graduation 1969: I graduated "with Honor" on June 6, 1969 with an M.D. (Medicinae Doctor) degree from Baylor College of Medicine, extremely pleased and deeply relieved that I had weathered the difficult and rigorous program, and ready to continue on the long road ahead. We had started in September 1965 with 85 members in my entering class, and remarkably, although there had been some rotations in and out of my class, we graduated 85 new MDs at that ceremony. Thus I believe there was very little attrition in the BCM medical students. I was now "Doctor McGoodwin", though that would not yet go very far toward buying me a cup of coffee.
At the ceremony, we were administered the Oath of Hippocrates. It was an updated and somewhat watered-down version compared to the classic version (see References 3 and 4 below for a comparison of the two). Dr. Michael DeBakey presided at this ceremony.
The Priesthood and Ethics of Medicine: On taking this oath, I entered into what I have always regarded as a sacred priesthood of physicians, male and female, sworn to uphold the evolving code of conduct of this noble profession. It is a professional identification and a solemn obligation that I have always taken very seriously and have done my best to honor. (Of course, there are more recent and expanded compilations of the ethical obligations of physicians, such as the American Medical Association's 2001 Principles of Medical Ethics. The World Medical Association has developed even more elaborate policies embodied in such statements as the 1983 Declaration of Geneva and the International Code of Medical Ethics, as well as more recently updated declarations pertaining to human research, patient's rights, the abuse of the elderly, torture, privacy, biological weapons, etc.)
MD versus PhD Degrees: In subsequent years as I got to know a wider assortment of university-based PhDs, I came to realize that some academics value and respect an MD degree differently from a PhD on an imaginary scale of prestige and intellectual achievement. The MD degree and the education that leads to it carry some very pragmatic, trade-school-like connotations—being able to treat an infant with diarrhea, sewing up wounds, working out various human plumbing leaks and corroded pipe problems, etc. The PhD seemed to be regarded as clearer evidence of advanced thought, and perhaps had higher standing in some non-medical academic circles. While in the active practice of medicine, I tended to hover at a fuzzy boundary separating the acquiring of scholarly knowledge as an enjoyable and intellectual end in itself, and the much more pragmatic pursuit of practical knowledge furthering my medical service to humanity and earning an income.
Board Exams and Texas Medical Licensure: I had previously passed the Texas State Board Examination in the Basic Sciences in May 1967. I flew back to Texas from Denver on about Sunday June 22, 1969 in order to take the Texas State Board of Medical Examiners written examination given in Fort Worth c. June 23 – June 25, 1969. I stayed in the Blackstone Hotel, built in 1929. I passed this exam, making the "Honor Roll of Examinees", and was awarded a license to practice Medicine and Surgery in Texas on August 27, 1969. Of course, I had insufficient training to actually go into practice, but it was nice to know that I could have hung out a shingle if I had wanted to, and it always gave me great pride to have this first medical license. (I kept my Texas license in force for 35 years, but in 2004 decided I could no longer afford to keep paying the renewal costs, by then exceeding $500 annually, and reluctantly let it lapse.)
(1) LA Geddes, LE Baker, MC McGoodwin. "The Relationship
Between Electrode Area and Amplifier Input Impedance in Recording Muscle Action
Potentials" Med and Biol. Engin. 5:561, 1967.
(2) The Staff of Asclepius (Aesculapian) versus The Caduceus of Hermes: The Staff of Asclepius (Æsclepius, Asklepios)
is the correct or traditional symbol of medicine, and (as depicted on
the cover of our BCM annuals), the Aesculapian consists of a single serpent encircling a tree limb or
staff. Asclepius was probably a skilled physician who practiced in
Greece around 1200 BCE (and is mentioned in Homer's Iliad), but also became a
mythological figure associated with the god of Healing. The symbol may have originated with the practice of extracting the large
parasitic guinea worm (Dracunculus medinensis) from the skin of its victim by cutting over the worm's path
in the skin and winding it gradually up on a stick. Eventually, the
rod and serpent emerged as the independent symbol of medicine, the Asclepian or
Aesculapian staff. I am pleased to see that my medical school had its
classical symbology correct, and was not seduced by the more symmetrical and
visually elegant but much disparaged two-serpented symbol, the Caduceus of
Hermes, used by drug
companies and the US Army, etc. to symbolize medicine.
See http://drblayney.com/Asclepius.html,
accessed 24 March 2009.
(3) The Updated Oath of Hippocrates, which we swore to in our graduation
ceremony: "I do solemnly swear, by whatever I hold most sacred: That I will
be loyal to the profession of medicine and just and generous to its members;
That I will lead my life and practice my profession in uprightness and honor;
That into whatsoever house I shall enter, it shall be for the good of the sick
to the utmost of my power, holding myself far aloof from wrong, from corruption,
from the tempting of others to vice; That I will exercise my profession solely
for the cure of my patients, and will give no drug, perform no operation, for a
criminal purpose, even if solicited; far less suggest it. That whatsoever
I shall see or hear of the lives of men which is not fitting to be spoken, I
will keep inviolably secret. These things I do swear. And now,
should I be true to this, my oath, may prosperity and good repute be ever mine;
the opposite, should I prove myself forsworn."
(4) The Original Oath of Hippocrates of Antiquity: "I swear by Apollo the Physician and Asclepius and Hygeia and Panaceia and all the gods and goddesses, making them my witnesses, that I will fulfill according to my ability and judgment this oath and this covenant:
To hold him who has taught me this art as equal to my parent and to live my life in partnership with him, and if he is in need of money to give him a share of mine, and to regard his offspring as equal to my brothers in male lineage and to teach them this art—if they desire to learn it—without fee and covenant; to give share of precepts and oral instruction and all other learning to my sons and to the sons of him who has instructed me and to pupils who have signed the covenant and have taken an oath according to the medical law, but to no one else.
I will apply dietetic measure for the benefit of the sick according to my ability and judgment; I will keep them from harm and injustice.
I will neither give a deadly drug to anybody if asked for it, nor will I make a suggestion to this effect.
Similarly I will not give a woman an abortive remedy.
In purity and in holiness I will guard my life and my art. I will not use the knife, not even on sufferers from stone, but will withdraw in favor of such men as are engaged in this work.
Whatever houses I may visit, I will come for the benefit of the sick, remaining free of all intentional injustice, of all mischief and in particular of sexual relations with both female and male persons, be they free or slaves.
What I may see or hear in the course of the treatment or even outside of the treatment in regard to the life of men, which on no account one must spread abroad, I will keep to myself holding such things shameful to be spoken about.
If I fulfill this oath and do not violate it, may it be granted to me to enjoy life and art, being honored with fame among all men for all time to come; if I transgress it and swear falsely, may the opposite be my lot."
Translated 1943 by Ludwig Edelstein,
See http://www.hsl.virginia.edu/historical/artifacts/antiqua/hippocrates.cfm, accessed
24 March 2009
(5) Collected writings of Hippocrates. On Digital Hippocrates, see http://daedalus.umkc.edu/hippocrates/, accessed 24 March 2009
(6) Chandler S. Robbins, Bertel Bruun, and Herbert S. Zim, Birds of
North America, Golden Press, 1966.
(7) Dee Brown, Bury My Heart At Wounded Knee: An Indian History of the
American West, Holt, Rinehart, and Winston, 1970.
(8) Alvin M. Josephy, Jr., The Indian Heritage of America, Alfred A.
Knopf, 1969.
(9) CDC historical published reports on the hazards of smoking, see http://www.cdc.gov/tobacco/data_statistics/sgr/index.htm,
accessed 24 March 2009.
(10) I Corinthians
13: This text celebrates benevolent or divine Love: αγαπη in Greek (shown here without diacritics), transliterated as agape, translated as Love or Charity in English, caritas in Latin, Liebe in German, amor or caridad in Spanish, and amour or charité in French. To most people, faith, hope and love are all important, but indeed "the greatest of these is love".